UnitedHealth to Require Drug Rebates Go to Consumers
12 Março 2019 - 7:29AM
Dow Jones News
By Anna Wilde Mathews
UnitedHealth Group Inc. said it would significantly expand a
change to how it handles rebates from drugmakers by requiring new
employer clients to pass them on to people who take the
medications.
The move will apply to employers that sign new contracts after
Jan. 1, 2020, but UnitedHealth will grandfather in existing clients
that chose a different setup. The new shift will involve employers
that begin using UnitedHealth's pharmacy-benefit manager, OptumRx,
including those that are self-insured, which is the vast majority
of large companies.
Drugmakers routinely pay rebates to insurers and
pharmacy-benefit managers to offset the full list price of
brand-name drugs. The companies use the rebates in a variety of
ways. Often, they are passed along to employer clients, which may
use them to reduce premiums for all workers, or defray their own
costs.
The move goes further than other major pharmacy-benefit
managers, which haven't made it mandatory to pass rebates on to
consumers, according to UnitedHealth and industry consultants. The
Trump administration has proposed a parallel approach that would
affect Medicare and Medicaid plans, which pharmacy-benefit managers
have generally opposed.
"We're focused on making sure the value we're negotiating on
behalf of our clients is passed on to the consumer," said John
Prince, chief executive of OptumRx. The move to make the shift
mandatory for new clients "is a huge statement to the market," he
said. UnitedHealth officials say the employer-plan situation is
different from Medicare, where shifting the rebate treatment could
force up premiums significantly.
UnitedHealth this year switched to passing along rebates
directly to consumers under certain employer plans offered by its
insurance arm, UnitedHealthcare, now affecting about nine million
people.
The topic of rebates--along with the opaque process of setting
prices for drugs in general--is currently under a bright spotlight,
with pharmaceutical executives in a recent congressional hearing
blaming the practices of insurers and pharmacy-benefit managers for
driving prices higher.
On the other side, health plans and benefit managers have said
they rein in costs by negotiating with drugmakers, including by
winning rebates that could be used to reduce premiums.
But critics, including Trump administration officials, say the
rebates should flow directly to the consumers who take the affected
medications to reduce their out-of-pocket charges. UnitedHealth
said its existing program to pass through rebates has lowered costs
for affected consumers by $130 per prescription on average and
increased their adherence to medication regimens.
A growing share of large employers pass along rebates to
patients who take the affected drugs, according to a survey by the
National Business Group on Health. Of the large employers surveyed,
20% were doing it in 2018, another 7% said they planned to start
this year and an additional 31% were considering a shift in 2020 or
2021. Brian Marcotte, CEO of the employer group, said he believed
the shift to passing rebates along to consumers "is the direction
everything is going."
Still, UnitedHealth risks pushback from employers that want to
use rebates in other ways. "Some employers won't like it,
absolutely," said Nadina Rosier, who is head of the pharmacy
practice at advisory firm Willis Towers Watson. "They want
flexibility to manage the benefit in the way they see fit, and the
goal is to drive to lowest net cost."
David Dross, leader of the pharmacy practice at Mercer, a
consulting unit of Marsh & McLennan, said some employers might
want the freedom to handle rebates the way they want and "they
might base their decision about a PBM on that."
Daniel J. Schumacher, president of UnitedHealthcare, said there
is a "potential risk" in making the rebate approach mandatory, but
"we think it's a risk worth taking," with major benefits
particularly for consumers who take high-cost medications.
Write to Anna Wilde Mathews at anna.mathews@wsj.com
(END) Dow Jones Newswires
March 12, 2019 06:14 ET (10:14 GMT)
Copyright (c) 2019 Dow Jones & Company, Inc.
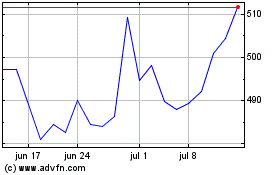
UnitedHealth (NYSE:UNH)
Gráfico Histórico do Ativo
De Mar 2024 até Abr 2024
UnitedHealth (NYSE:UNH)
Gráfico Histórico do Ativo
De Abr 2023 até Abr 2024
