Press Release: ASH: Sarclisa combinations demonstrated significant
benefits in newly diagnosed multiple myeloma patients
ASH: Sarclisa combinations demonstrated
significant benefits in newly diagnosed multiple myeloma
patients
- New analysis from the IMROZ phase 3
study of Sarclisa-VRd demonstrated higher and sustained MRD
negativity rates in transplant-ineligible NDMM patients
versus VRd alone
- New detailed results from the
GMMG-HD7 phase 3 study of Sarclisa-RVd induction therapy resulted
in a significant and clinically meaningful PFS benefit with deeper
MRD negativity in transplant-eligible NDMM patients
- Results support the benefit of
Sarclisa-based combinations to patients in the front-line setting
and the ongoing use of MRD negativity as a potential surrogate
endpoint for PFS in MM research
Paris, December 9, 2024. New
data from three oral presentations, which demonstrated significant
clinical benefit with Sarclisa-based quadruplets in newly diagnosed
multiple myeloma (NDMM) patients were featured at the 66th American
Society of Hematology (ASH) Annual Meeting & Exposition in San
Diego, CA, US. The presentations, including results from the IMROZ
and German-speaking Myeloma Multicenter Group (GMMG)-HD7 phase 3
studies, showcased deep and durable responses and improved
long-term outcomes with Sarclisa when added to current
standard-of-care NDMM regimens.
Dietmar Berger, MD,
PhD
Chief Medical Officer, Global Head of Development at Sanofi
“An important part of our approach to scientific innovation in
oncology is identifying synergistic combinations, which may allow
us to impact numerous unmet needs with a single therapy and expand
the pool of patients who could one day benefit from our medicines.
Results from key studies evaluating Sarclisa combinations further
reinforce our confidence in this strategy and speak to the
potential benefit of Sarclisa as a backbone therapy for newly
diagnosed multiple myeloma, regardless of transplant
eligibility.”
Additional IMROZ phase 3 study analysis
evaluating MRD in transplant-ineligible (TI) NDMM patients
The IMROZ phase 3 study demonstrated that Sarclisa in combination
with standard-of-care bortezomib, lenalidomide and dexamethasone
(VRd), followed by Sarclisa-Rd, improved progression-free survival
(PFS) and led to a rapid and greater depth of response compared to
VRd alone, as shown by minimal residual disease (MRD) negativity
rate over time, in TI NDMM patients. MRD negativity represents a
measure of malignant cells left in the bone marrow after treatment
and has been increasingly used as a surrogate endpoint for PFS in
MM research. Numerous independent studies have shown a correlation
between MRD negativity, deeper treatment responses and improved
long-term outcomes.
Sarclisa-VRd demonstrated a consistent benefit
at every time point up to 60 months and led to the highest MRD
negativity rate of a NDMM regimen with a VRd backbone, when
evaluating exclusively TI patients.
- Higher MRD
negativity rates were observed at both the end of initiation and
during maintenance, with 58.1% of patients in the
intention-to-treat (ITT) population treated with Sarclisa-VRd
achieving MRD negativity versus 43.6% of patients in the
control arm (OR 1.79; 95% CI: 1.22 to 2.63; p=0.0014).
-
In addition, patients treated with Sarclisa-VRd were significantly
less likely to lose MRD negativity status post-induction, with
only 12.3% of patients converting to MRD-positive status
during maintenance (at 36 months), compared to 34.8% of
patients in the control arm.
- Sustained MRD negativity
rates at ≥24 and ≥36 months were also two-to-threefold higher with
Sarclisa-VRd compared to VRd (35.8% vs 13.3% and 25.7% vs
7.2%, respectively) at 10-5 sensitivity threshold, with
higher rates also observed in the experimental arm at
10-6 sensitivity threshold. The deep responses observed
with Sarclisa-VRd ultimately translated into an early PFS benefit
that was maintained over time.
- The safety and tolerability of
Sarclisa observed in this study was consistent with the established
safety profile of Sarclisa and VRd with no new safety signals
observed.
Robert Orlowski, MD,
PhD
Florence Maude Thomas Cancer Research Professor at The University
of Texas MD Anderson Cancer Center
“MRD negativity has long been used to infer deeper responses
and improved outcomes in multiple myeloma research, but few studies
have evaluated sustained MRD negativity beyond one year. In the
latest analysis from the IMROZ study, one of the longest to
evaluate MRD negativity with a CD38-based quadruplet, newly
diagnosed transplant-ineligible patients treated with
isatuximab-VRd were more likely to achieve this threshold compared
to those receiving VRd alone and maintain it as long as three
years. When viewed in tandem with earlier findings highlighting the
significant progression-free survival benefit from IMROZ, these
data reinforce the potential of isatuximab to generate deep and
durable improvements in clinical outcomes throughout treatment when
added to the standard-of-care regimen.”
New key results from the GMMG-HD7
study in transplant-eligible (TE) NDMM
New data from the induction part of the GMMG-HD7 phase 3 study were
featured across two oral presentations at ASH. GMMG-HD7 is an
investigational, pivotal, randomized, open-label, multicenter,
2-part phase 3 study evaluating Sarclisa in combination with RVd
versus RVd induction followed by post-transplant re-randomization
to Sarclisa plus lenalidomide versus lenalidomide maintenance in TE
NDMM patients. The following results, which were simultaneously
published in the Journal of Clinical Oncology, were
reported for Sarclisa-RVd compared to RVd in the first part:
- Higher MRD
negativity rates were observed at the end of initiation (18 weeks)
as assessed as a primary endpoint, with 50.1% of patients
in the ITT population treated with Sarclisa-RVd achieving MRD
negativity versus 35.6% of patients in the control arm (OR
1.83; 95% CI: 1.34 to 2.51; p<0.001).
- 30% reduction in the risk
of disease progression or death observed at a median
follow-up of 47 months from first randomization in patients treated
with Sarclisa-RVd during induction, regardless of the maintenance
therapy received (HR 0.70; 95% CI 0.52-0.95; stratified log-rank
p=0.0184).
- Three-year PFS rates in the
Sarclisa-RVd arm were 83% compared to 75% in the control
arm.
- Additionally, 53.1% of
patients receiving Sarclisa-RVd experienced continued MRD
negativity (compared to 38% in the control arm), defined
as MRD negativity persisting from post-induction to
post-transplant, which was consistent with a prolonged PFS benefit
(OR 1.84; 95% CI: 1.28-2.63; p=0.0008).
The safety and tolerability in this study were
consistent with the established safety profile of Sarclisa and RVd
with no new safety signals observed.
GMMG-HD7 is the first and only phase 3 study to
demonstrate a deep and rapid response with an anti-CD38-based
induction regimen in TE NDMM patients, regardless of maintenance
therapy, alongside a statistically significant MRD negativity
benefit post-induction, without consolidation. Additionally, the
data showed the highest post-induction and post-transplant MRD
negativity rates of any CD38 monoclonal antibody using RVd as a
backbone in TE NDMM. The results add to the growing body of
clinical evidence supporting the use of Sarclisa in the front-line
setting.
Hartmut Goldschmidt,
MD
President of GMMG, Professor of Medicine at the Heidelberg
University Hospital (UKHD), Germany and principal investigator of
the study
“Successful induction therapy prior to autologous stem cell
transplant is critical to achieving optimal outcomes in front-line
multiple myeloma treatment. In the GMMG-HD7 study, we observed a
significant and sustained progression-free survival benefit when
adding isatuximab to the current standard-of-care induction
regimen, reinforcing the potential of this quadruplet when used
prior to transplant, regardless of the maintenance
therapy.”
Advancing Sarclisa combinations in
hematologic malignancies
A fourth oral presentation at ASH featured interim results from the
investigational ISAMYP phase 2 study in AL amyloidosis, another
rare disease. Results showed the addition of Sarclisa to
pomalidomide, and dexamethasone (Pd) resulted in rapid
hematological responses in patients with relapsed AL amyloidosis,
who experienced suboptimal response to previous therapy or at
relapse. AL amyloidosis is a rare plasma cell disorder associated
with particularly poor outcomes in the later stages of the disease.
Although recent treatment advancements have helped improve outcomes
for certain patient segments, unmet needs continue to exist,
particularly for frail or TI populations.
The safety and efficacy of Sarclisa in
combination with Pd for AL amyloidosis has not been evaluated by
any regulatory authority.
About the IMROZ study
The randomized, multi-center, open label IMROZ phase 3 study
enrolled 446 patients with TI NDMM across 21 countries and 96
centers. During the study, Sarclisa was administered through an
intravenous infusion at a dose of 10 mg/kg once weekly for five
weeks during first 42-day cycle and once every two weeks in cycles
2 to 4 in combination with subcutaneous bortezomib, oral
lenalidomide and intravenous or oral dexamethasone. Then Sarclisa
was administered every 2 weeks from cycle 5 to 17 and every 4 weeks
in cycles 18+ during 28-day cycles in combination with lenalidomide
and dexamethasone at the standard dose, until disease progression,
unacceptable toxicity, or patient’s decision to stop the study
treatment. The primary endpoint of IMROZ is PFS. Key secondary
endpoints include complete response rate, MRD negativity rate for
patients with a complete response, very good partial response or
better rate, and overall survival. Other secondary endpoints are
overall response rate, time to progression, duration of response,
time to first response, time to best response, PFS on next line of
therapy, PFS by MRD status, sustained MRD negativity greater than
or equal to 12 months rate, safety, pharmacokinetic profile,
immunogenicity, disease-specific and generic health-related quality
of life, disease and treatment-related symptoms, health state
utility, and health status.
In September 2024, Sarclisa was approved in the
US in combination with VRd as a front-line treatment option for
adult patients with NDMM who are not eligible for ASCT, based on
results from the IMROZ phase 3 study. In November 2024, the
European Medicines Agency (EMA)’s Committee for Medicinal Products
for Human Use (CHMP) adopted a positive opinion recommending the
approval of Sarclisa-VRd for the treatment of adult patients with
NDMM who are ineligible for ASCT. Additionally, applications for
this indication are currently under regulatory review in Japan and
China.
About the GMMG-HD7 study
GMMG-HD7 is an investigational, pivotal, randomized, open-label,
multicenter, 2-part phase 3 study evaluating Sarclisa in
combination with RVd versus RVd induction followed by
post-transplant re-randomization to Sarclisa plus lenalidomide
versus lenalidomide maintenance in TE NDMM patients. The
GMMG-initiated study is being conducted in close collaboration with
Sanofi based on jointly defined research. Sanofi provided financial
support to GMMG for this study. In December 2021, Sanofi and GMMG
shared results from part one, which met the primary endpoint of MRD
negativity after induction therapy and before transplant in NDMM
patients.
The study enrolled 662 patients with TE NDMM
across 67 sites in Germany. In the first part of the study, all
participants were equally randomized to receive three 42-day cycles
of RVd in both arms of the study, while Sarclisa was added to only
one study arm. In the second part of the study, patients were
re-randomized post-transplant to receive Sarclisa plus lenalidomide
or lenalidomide alone as maintenance therapy. During the study,
Sarclisa was administered through an intravenous infusion at a dose
of 10 mg/kg once weekly for the first four weeks of cycle one, then
every other week for the rest of the induction period.
MRD negativity was assessed by next-generation
flow cytometry (sensitivity of 1x10-5) after induction.
In the latest readout of the study, PFS for both Sarclisa plus RVd
as an induction therapy, regardless of maintenance treatment, and
Sarclisa plus lenalidomide as a maintenance regimen were measured
from first randomization.
GMMG-HD7 protocol defined the primary endpoints
of MRD negativity after induction treatment for the first part of
the study, and PFS following the second randomization after
transplant for part two of the study, in which Sarclisa was added
to lenalidomide maintenance, with the latter primary endpoint
anticipated to be available later. The key secondary endpoint for
the first part of the study was PFS from first randomization.
Additional secondary endpoints included rates of complete response
after induction, and intensification, overall survival, and
safety.
The use of Sarclisa in combination with RVd is
investigational and has not been evaluated by any regulatory
authority. Submission of an application for this combination in the
EU is anticipated in the coming months.
About Sarclisa
Sarclisa (isatuximab) is a CD38 monoclonal antibody that binds to a
specific epitope on the CD38 receptor on MM cells, inducing
distinct antitumor activity. It is designed to work through
multiple mechanisms of action including programmed tumor cell death
(apoptosis) and immunomodulatory activity. CD38 is highly and
uniformly expressed on the surface of MM cells, making it a target
for antibody-based therapeutics such as Sarclisa. In the US, the
non-proprietary name for Sarclisa is isatuximab-irfc, with irfc as
the suffix designated in accordance with nonproprietary naming of
biological products guidance for industry issued by the US FDA.
Currently Sarclisa is approved in more than 50
countries, including the US and EU, across two indications;
Sarclisa is approved under an additional indication in the US.
Based on the ICARIA-MM phase 3 study, Sarclisa is approved in
combination with Pd for the treatment of patients with relapsed
refractory MM (R/R MM) who have received ≥2 prior therapies,
including lenalidomide and a proteasome inhibitor and who
progressed on last therapy. Based on the IKEMA phase 3 study,
Sarclisa is also approved in 50 countries in combination with
carfilzomib and dexamethasone, including in the US for the
treatment of patients with R/R MM who have received 1–3 prior lines
of therapy and in the EU for patients with MM who have received at
least 1 prior therapy. In the US, Sarclisa is approved in
combination with VRd as a front-line treatment option for adult
patients with NDMM who are not eligible for ASCT, based on the
IMROZ phase 3 study. On November 14, 2024, the European Medicines
Agency (EMA)’s Committee for Medicinal Products for Human Use
(CHMP) adopted a positive opinion recommending the approval of
Sarclisa-VRd in this patient population. A final decision is
expected in the coming months.
Sanofi continues to advance Sarclisa as part of
a patient-centric clinical development program, which includes
several phase 2 and phase 3 studies across the MM treatment
continuum spanning six potential indications. In addition, the
company is evaluating a subcutaneous administration method for
Sarclisa in clinical studies. The safety and efficacy of Sarclisa
has not been evaluated by any regulatory authority outside of its
approved indications and methods of delivery.
In striving to become the number one
immunoscience company globally, Sanofi remains committed to
advancing oncology innovation. Through focused strategic decisions
the company has reshaped and prioritized its pipeline, leveraging
its expertise in immunoscience to drive progress. Efforts are
centered on difficult-to-treat often rare cancers such as select
hematologic malignancies and solid tumors with critical unmet
needs, including multiple myeloma, acute myeloid leukemia, certain
types of lymphomas, as well as gastrointestinal and lung
cancers.
For more information on Sarclisa clinical
studies, please visit www.clinicaltrials.gov.
About the German-speaking Myeloma
Multicenter Group (GMMG)
GMMG is the largest study group focusing on MM in Germany, with
headquarters based in Heidelberg. Within the last 20+ years, the
GMMG study group has performed numerous studies including five
randomized, multicenter phase 3 studies with 4,000 patients
enrolled from about 90 participating and co-treating centers
throughout Germany. The overall goal of GMMG is to generate
improved therapies for myeloma patients through the development and
testing of novel and personalized, genome- and signaling-driven
treatment strategies. The GMMG has set itself the goal of achieving
further approvals for effective antibody-based drug combinations
for the first-line treatment of myeloma patients, in which
antibody-based treatment regimens have been integrated into seven
GMMG study concepts (CONCEPT, DANTE, DADA, HD6, HD7, HD8, HD9 and
HD10).
About Sanofi
We are an innovative global healthcare company, driven by one
purpose: we chase the miracles of science to improve people’s
lives. Our team, across the world, is dedicated to transforming the
practice of medicine by working to turn the impossible into the
possible. We provide potentially life-changing treatment options
and life-saving vaccine protection to millions of people globally,
while putting sustainability and social responsibility at the
center of our ambitions.
Sanofi is listed on EURONEXT: SAN and NASDAQ: SNY
Media Relations
Sandrine Guendoul | +33 6 25 09 14 25
| sandrine.guendoul@sanofi.com
Evan Berland | +1 215 432 0234 |
evan.berland@sanofi.com
Nicolas Obrist | +33 6 77 21 27 55 |
nicolas.obrist@sanofi.com
Léo Le Bourhis | + 33 6 75 06 43 81 |
leo.lebourhis@sanofi.com
Victor Rouault | +33 6 70 93 71 40
| victor.rouault@sanofi.com
Timothy Gilbert | +1 516 521 2929 |
timothy.gilbert@sanofi.com
Investor Relations
Thomas Kudsk Larsen |+44 7545 513 693 |
thomas.larsen@sanofi.com
Alizé Kaisserian | +33 6 47 04 12 11 |
alize.kaisserian@sanofi.com
Felix Lauscher | +1 908 612
7239 | felix.lauscher@sanofi.com
Keita Browne | +1 781 249 1766 |
keita.browne@sanofi.com
Nathalie Pham | +33 7 85 93 30 17 |
nathalie.pham@sanofi.com
Tarik Elgoutni | +1 617 710 3587 |
tarik.elgoutni@sanofi.com
Thibaud Châtalet | +33 6 80 80 89 90 |
thibaud.chatalet@sanofi.com
This press release contains forward-looking
statements as defined in the Private Securities Litigation Reform
Act of 1995, as amended. Forward-looking statements are statements
that are not historical facts. These statements include projections
and estimates regarding the marketing and other potential of the
product, or regarding potential future revenues from the product.
Forward-looking statements are generally identified by the words
“expects”, “anticipates”, “believes”, “intends”, “estimates”,
“plans” and similar expressions. Although Sanofi’s management
believes that the expectations reflected in such forward-looking
statements are reasonable, investors are cautioned that
forward-looking information and statements are subject to various
risks and uncertainties, many of which are difficult to predict and
generally beyond the control of Sanofi, that could cause actual
results and developments to differ materially from those expressed
in, or implied or projected by, the forward-looking information and
statements. These risks and uncertainties include among other
things, unexpected regulatory actions or delays, or government
regulation generally, that could affect the availability or
commercial potential of the product, the fact that product may not
be commercially successful, the uncertainties inherent in research
and development, including future clinical data and analysis of
existing clinical data relating to the product, including post
marketing, unexpected safety, quality or manufacturing issues,
competition in general, risks associated with intellectual property
and any related future litigation and the ultimate outcome of such
litigation, and volatile economic and market conditions, and the
impact that pandemics or other global crises may have on us, our
customers, suppliers, vendors, and other business partners, and the
financial condition of any one of them, as well as on our employees
and on the global economy as a whole. The risks and uncertainties
also include the uncertainties discussed or identified in the
public filings with the SEC and the AMF made by Sanofi, including
those listed under “Risk Factors” and “Cautionary Statement
Regarding Forward-Looking Statements” in Sanofi’s annual report on
Form 20-F for the year ended December 31, 2023. Other than as
required by applicable law, Sanofi does not undertake any
obligation to update or revise any forward-looking information or
statements.
All trademarks mentioned in this press
release are the property of the Sanofi group.


Sanofi (EU:SAN)
Gráfico Histórico do Ativo
De Fev 2025 até Mar 2025
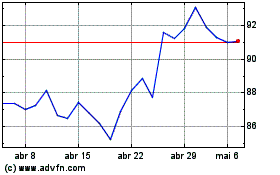
Sanofi (EU:SAN)
Gráfico Histórico do Ativo
De Mar 2024 até Mar 2025
