Treatment effects sustained through long-term
follow-up of beyond 10 years in the earliest treated patients
(n=2); 81% of participants have >5 years of follow-up
bluebird bio, Inc. (Nasdaq: BLUE) today announced updated data
from patients with beta-thalassemia who require regular blood
transfusions treated with betibeglogene autotemcel (beti-cel,
approved commercially as ZYNTEGLO™) in clinical studies. The data
was presented today at the 66th American Society of Hematology
(ASH) Annual Meeting and Exposition.
“Updated follow-up data of up to 10 years showed that patients
treated with beti-cel in clinical trials experienced durable
transfusion independence and normal or near-normal hemoglobin,
regardless of genotype and age, and a continued favorable safety
profile”, said Richard Colvin, M.D., Ph.D., chief medical officer,
bluebird bio. “We are deeply grateful for the ongoing commitment of
our investigators, patients, and study participants. Our collective
efforts are not only advancing the field of gene therapy but also
providing new hope and possibilities for individuals with severe
genetic diseases."
“Data at ASH demonstrate the durability of beti-cel through 10
years of long-term follow-up, giving additional confidence in that
the transformational outcomes observed in parent studies are
sustained over time,” said Alexis Thompson, MD, MPH, Chief of the
Division of Hematology at Children’s Hospital of Philadelphia,
which is a Qualified Treatment Center for ZYNTEGLO. “These
long-term data demonstrate beti-cel’s continued positive impact on
iron management outcomes over time, which can help inform treatment
decisions by clinicians who are now using this therapy in the
real-world setting.”
Betibeglogene Autotemcel (beti-cel) Gene Addition Therapy
results in durable Hemoglobin A (HbA) Production with up to 10
Years of Follow-Up in Participants with Transfusion-Dependent
β-Thalassemia (Poster #2194)
Long-term outcomes with beti-cel in adult and pediatric patients
with TDT were presented in a poster session. The data focused on 63
adult and pediatric study participants who had received beti-cel in
a Phase 1/2 or Phase 3 study. Two participants had 10 years of
follow-up, and 51 (81.0%) participants had 5 or more years of
follow-up. Additionally, iron status was assessed in study
participants who achieved TI and discontinued chelation therapy.
Results showed that majority of participants treated with beti-cel
achieved TI. All participants achieved platelet and neutrophil
engraftment. Specific findings showed:
- Of 63 patients, 52 (90.2% in Phase 3 studies and 68.2% in Phase
1/2 studies) achieved TI. All except one patient maintained TI
through last follow-up. The median weighted average hemoglobin
during TI was 10.2 mg/dL for Phase 1/2 studies and 11.2 mg/dL for
Phase 3 studies. Achievement and maintenance of TI and median
weighted average hemoglobin were similar across ages and
genotypes.
- Study participants treated with beti-cel who achieved and
maintained TI demonstrated effective restoration of iron
homeostasis over time and reduced iron management burden. Among
participants who achieved TI, improvements in serum ferritin and
liver iron concentration were sustained through month 60. 28/37
(75.7%) study participants who achieved TI in Phase 3 studies are
no longer undergoing iron chelation therapy.
- Both adult and pediatric health-related quality of life scores
(HRQoL) remained above the normative population mean up to 60
months. All 26 participants who achieved TI and completed a
questionnaire reported an overall benefit with beti-cel.
- The safety profile was consistent with known side effects of
hematopoietic stem cell collection and the busulfan conditioning
regimen. None of the study participants had a fatal event. No
beti-cel–related serious adverse events were reported more than 2
years after infusion through last follow-up. No malignancies,
insertional oncogenesis or vector-derived replication-competent
lentivirus were reported in any study participants.
Beti-cel was approved by the FDA in August 2022 and is
commercially available in the United States as ZYNTEGLO.
About ZYNTEGLO® (betibeglogene autotemcel) or
beti-cel
ZYNTEGLO is a first-in-class, one-time ex-vivo LVV gene therapy
approved for the treatment of beta-thalassemia in adult and
pediatric patients who require regular red blood cell transfusions.
ZYNTEGLO works by adding functional copies of a modified form of
the beta-globin gene (βA-T87Q-globin gene) into a patient’s own
hematopoietic (blood) stem and progenitor cells to enable the
production of a modified functional adult hemoglobin (HbAT87Q).
Once a patient has the βA-T87Q-globin gene, they have the potential
to increase ZYNTEGLO-derived adult hemoglobin (HbAT87Q) and total
hemoglobin to normal or near normal levels that can eliminate the
need for regular red blood cell (RBC) transfusions.
Indication
ZYNTEGLO is indicated for the treatment of adult and pediatric
patients with beta-thalassemia who require regular red blood cell
(RBC) transfusions.
Important Safety Information
Delayed Platelet Engraftment
Delayed platelet engraftment has been observed with ZYNTEGLO
treatment. Bleeding risk is increased prior to platelet engraftment
and may continue after engraftment in patients with prolonged
thrombocytopenia; 15% of patients had ≥ Grade 3 decreased platelets
on or after Day 100.
Patients should be made aware of the risk of bleeding until
platelet recovery has been achieved. Monitor patients for
thrombocytopenia and bleeding according to standard guidelines.
Conduct frequent platelet counts until platelet engraftment and
platelet recovery are achieved. Perform blood cell count
determination and other appropriate testing whenever clinical
symptoms suggestive of bleeding arise.
Risk of Neutrophil Engraftment Failure
There is a potential risk of neutrophil engraftment failure
after treatment with ZYNTEGLO. Neutrophil engraftment failure is
defined as failure to achieve three consecutive absolute neutrophil
counts (ANC) ≥ 500 cells/microliter obtained on different days by
Day 43 after infusion of ZYNTEGLO. Monitor neutrophil counts until
engraftment has been achieved. If neutrophil engraftment failure
occurs in a patient treated with ZYNTEGLO, provide rescue treatment
with the back-up collection of CD34+ cells.
Risk of Insertional Oncogenesis
There is a potential risk of LVV mediated insertional
oncogenesis after treatment with ZYNTEGLO.
Patients treated with ZYNTEGLO may develop hematologic
malignancies and should be monitored lifelong. Monitor for
hematologic malignancies with a complete blood count (with
differential) at Month 6 and Month 12 and then at least annually
for at least 15 years after treatment with ZYNTEGLO, and
integration site analysis at Months 6, 12, and as warranted.
In the event that a malignancy occurs, contact bluebird bio at 1
833-999-6378 for reporting and to obtain instructions on collection
of samples for testing.
Hypersensitivity Reactions
Allergic reactions may occur with the infusion of ZYNTEGLO. The
dimethyl sulfoxide (DMSO) in ZYNTEGLO may cause hypersensitivity
reactions, including anaphylaxis.
Anti-retroviral and Hydroxyurea Use
Patients should not take prophylactic HIV anti-retroviral
medications or hydroxyurea for at least one month prior to
mobilization, or for the expected duration for elimination of the
medications, and until all cycles of apheresis are completed. If a
patient requires anti-retrovirals for HIV prophylaxis, then confirm
a negative test for HIV before beginning mobilization and apheresis
of CD34+ cells.
Interference with Serology Testing
Patients who have received ZYNTEGLO are likely to test positive
by polymerase chain reaction (PCR) assays for HIV due to integrated
BB305 LVV proviral DNA, resulting in a false-positive test for HIV.
Therefore, patients who have received ZYNTEGLO should not be
screened for HIV infection using a PCR‑based assay.
Adverse Reactions
The most common non-laboratory adverse reactions (≥20%) were
mucositis, febrile neutropenia, vomiting, pyrexia, alopecia,
epistaxis, abdominal pain, musculoskeletal pain, cough, headache,
diarrhea, rash, constipation, nausea, decreased appetite,
pigmentation disorder, and pruritus. The most common Grade 3 or 4
laboratory abnormalities (>50%) include neutropenia,
thrombocytopenia, leukopenia, anemia, and lymphopenia.
Drug Interactions
Drug-drug interactions between iron chelators and the
myeloablative conditioning agent must be considered. Iron chelators
should be discontinued at least 7 days prior to initiation of
conditioning. The prescribing information for the iron chelator(s)
and the myeloablative conditioning agent should be consulted for
the recommendations regarding co-administration with CYP3A
substrates.
Some iron chelators are myelosuppressive. After ZYNTEGLO
infusion, avoid use of these iron chelators for 6 months. If iron
chelation is needed, consider administration of
non-myelosuppressive iron chelators. Phlebotomy can be used in lieu
of iron chelation, when appropriate.
Pregnancy/Lactation
Advise patients of the risks associated with conditioning
agents, including on pregnancy and fertility. ZYNTEGLO should not
be administered to women who are pregnant, and pregnancy after
ZYNTEGLO infusion should be discussed with the treating
physician.
ZYNTEGLO is not recommended for women who are breastfeeding, and
breastfeeding after ZYNTEGLO infusion should be discussed with the
treating physician.
Females and Males of Reproductive Potential
A negative serum pregnancy test must be confirmed prior to the
start of mobilization and re-confirmed prior to conditioning
procedures and before ZYNTEGLO administration.
Women of childbearing potential and men capable of fathering a
child should use an effective method of contraception (intra
uterine device or combination of hormonal and barrier
contraception) from start of mobilization through at least 6 months
after administration of ZYNTEGLO.
Advise patients of the option to cryopreserve semen or ova
before treatment if appropriate.
Please see full Prescribing Information for
ZYNTEGLO.
About bluebird bio, Inc.
bluebird bio is pursuing curative gene therapies to give
patients and their families more bluebird days.
Founded in 2010, bluebird has been setting the standard for gene
therapy for more than a decade—first as a scientific pioneer and
now as a commercial leader. bluebird has an unrivaled track record
in bringing the promise of gene therapy out of clinical studies and
into the real-world setting, having secured FDA approvals for three
therapies in under two years. Today, we are proving and scaling the
commercial model for gene therapy and delivering innovative
solutions for access to patients, providers, and payers.
With a dedicated focus on severe genetic diseases, bluebird has
the largest and deepest ex-vivo gene therapy data set in the field,
with industry-leading programs for sickle cell disease,
β-thalassemia and cerebral adrenoleukodystrophy. We custom design
each of our therapies to address the underlying cause of disease
and have developed in-depth and effective analytical methods to
understand the safety of our lentiviral vector technologies and
drive the field of gene therapy forward.
bluebird continues to forge new paths as a standalone commercial
gene therapy company, combining our real-world experience with a
deep commitment to patient communities and a people-centric culture
that attracts and grows a diverse flock of dedicated birds.
Forward-Looking Statements
This press release contains “forward-looking statements” within
the meaning of the Private Securities Litigation Reform Act of
1995. All statements that are not statements of historical facts
are, or may be deemed to be, forward-looking statements, such as
statements regarding the therapeutic potential of ZYNTEGLO. Such
forward-looking statements are based on historical performance and
current expectations and projections about bluebird’s future goals,
plans and objectives and involve inherent risks, assumptions and
uncertainties, including internal or external factors that could
delay, divert or change any of them in the next several years, that
are difficult to predict, may be beyond bluebird’s control and
could cause bluebird’s future goals, plans and objectives to differ
materially from those expressed in, or implied by, the statements.
No forward-looking statement can be guaranteed. Forward-looking
statements in this press release should be evaluated together with
the many risks and uncertainties that affect bluebird bio’s
business, particularly those identified in the risk factors
discussion in bluebird bio’s Annual Report on Form 10-K for the
year ended December 31, 2023, as updated by its subsequent
Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and
other filings with the SEC. These risks and uncertainties include,
but are not limited to: the risk that the efficacy and safety
results from bluebird’s prior and ongoing clinical trials will not
continue or be seen in the commercial context; the risk that there
is not sufficient patient demand or payer reimbursement to support
continued commercialization of ZYNTEGLO; the risk of insertional
oncogenic or other safety events associated with lentiviral vector,
drug product, or myeloablation, including the risk of hematologic
malignancy; and the risk that bluebird’s products, including
ZYNTEGLO, will not be successfully commercialized. The
forward-looking statements included in this document are made only
as of the date of this document and except as otherwise required by
applicable law, bluebird bio undertakes no obligation to publicly
update or revise any forward-looking statement, whether as a result
of new information, future events, changed circumstances or
otherwise.
View source
version on businesswire.com: https://www.businesswire.com/news/home/20241207259439/en/
Investors: Courtney O’Leary, 978-621-7347
coleary@bluebirdbio.com Media: Jess Rowlands,
857-299-6103 jess.rowlands@bluebirdbio.com
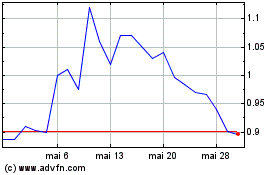
bluebird bio (NASDAQ:BLUE)
Gráfico Histórico do Ativo
De Nov 2024 até Dez 2024
bluebird bio (NASDAQ:BLUE)
Gráfico Histórico do Ativo
De Dez 2023 até Dez 2024
