Teva Pharmaceuticals, a U.S. affiliate of Teva Pharmaceutical
Industries Ltd. (NYSE and TASE: TEVA), and Sanofi today presented
new, detailed results from the RELIEVE UCCD Phase 2b study of
duvakitug (TEV’574/SAR447189), a human IgG1-λ2 monoclonal antibody
targeting TL1A, for the treatment of moderate-to-severe ulcerative
colitis (UC) and Crohn’s disease (CD), the two most common forms of
inflammatory bowel disease (IBD). These results were shared in two
oral presentations at the 20th Congress of the European Crohn’s and
Colitis Organisation (ECCO) in Berlin, Germany.1, 4
Ulcerative colitis
In the UC cohort of the RELIEVE UCCD study, 36%
(450 mg dose) and 48% (900 mg dose) of patients treated with
duvakitug achieved the primary endpoint of clinical remission
(mMS)* at week 14 compared to 20% treated with placebo;
placebo-adjusted rates were 16% (450 mg) and 27% (900 mg) (p=0.050
and 0.003, respectively).1-3
In addition, higher clinical remission rates
were observed for both doses of duvakitug versus placebo in both
advanced therapy (AT)-experienced and AT-naïve subgroups of
patients.
- AT-experienced:
29% (450 mg) and 36% (900 mg), with placebo-adjusted rates of 22%
(450 mg) and 29% (900 mg).
- AT-naïve: 39%
(450 mg) and 53% (900 mg), with placebo-adjusted rates of 12% (450
mg) and 26% (900 mg).1-3
Additional endpoints observed*:
- Clinical
response (mMS): 81% (450 mg) and 70% (900 mg) compared to 52%
treated with placebo.
- Endoscopic
improvement (MES): 45% (450 mg) and 50% (900 mg) compared to 23%
treated with placebo.
-
Histological-endoscopic mucosal improvement (HEMI): 30% (450 mg)
and 33% (900 mg) compared to 16% treated with placebo.1-3
“Patients, many of whom have spent years in a
recurring cycle of remission and relapse, have been waiting a long
time for better options in treating ulcerative colitis. We’re
highly encouraged by the significant treatment response, compared
to placebo seen in the study, both in advanced therapy naïve-and
experienced patients,” said Walter Reinisch, MD, PhD, Medical
University of Vienna, and lead investigator of the RELIEVE UCCD
study. “With this potential of duvakitug to reduce inflammation, we
could truly transform treatment for patients with IBD in a safe
manner.”
Crohn’s disease
In the CD cohort of the RELIEVE UCCD study, 26%
(450 mg) and 48% (900 mg) of patients with CD treated with
duvakitug achieved the primary endpoint of endoscopic response
(SES-CD)* compared to 13% on placebo; placebo-adjusted rates were
13% (450 mg) and 35% (900 mg) at week 14 (p=0.058 and <0.001,
respectively).
In addition, higher endoscopic response rates
were observed for both doses of duvakitug versus placebo in both
AT-experienced and -naïve subgroups of patients.
- AT-experienced:
11% (450 mg) and 48% (900 mg), with placebo-adjusted rates of 7%
(450 mg) and 44% (900 mg).
- AT-naïve: 47%
(450 mg) and 47% (900 mg), with placebo-adjusted rates of 25% (450
mg) and 25% (900 mg).2-4
Additional endpoints observed:
- Endoscopic
remission (SES-CD): 17% (450 mg) and 26% (900 mg) compared to 9%
treated with placebo.
- Clinical
remission (CDAI): 50% (450 mg) and 54% (900 mg) compared to 41%
treated with placebo.
- Clinical
response (CDAI): 61% (450 mg) and 62% (900 mg) compared to 41%
treated with placebo.
- Clinical
response (PRO2): 50% (450 mg) and 53% (900 mg) compared to 29%
treated with placebo.2-4
“Every day, I see patients with Crohn’s disease
who continue to suffer from the often-severe symptoms of the
disease despite available treatments,” said Vipul Jairath, MBChB,
DPhil, FRCP, FRCPC, Professor of Medicine in the Departments of
Medicine, Epidemiology and Biostatistics at Western University, and
lead investigator of the RELIEVE UCCD study. “The endoscopic
response rates seen in this study support the potential of
duvakitug as an effective new option for these who are in desperate
need of relief.”
RELIEVE UCCD safety data
summary
In both the UC and CD cohorts, duvakitug was
generally well tolerated with no emergent safety signals
observed.1-4 No dose dependent or adverse event (AE) pattern was
observed for treatment-related AEs, serious adverse events (SAEs),
AEs leading to discontinuation or adverse events of special
interest (AESIs).
Duvakitug is currently under clinical
investigation, and its efficacy and safety have not been evaluated
by any regulatory authority.
Teva Investor CallTeva will hold an investor
call and live webcast on Monday, February 24, 2025, at 8:00 a.m.
ET. During the conference call, Eric Hughes, MD, PhD, Executive
Vice President of Global R&D and Chief Medical Officer, and
external IBD key opinion leaders (KOLs) will discuss new data
presented for duvakitug (Anti-TL1A) positive Phase 2b results at
the 20th Annual Congress of the European Crohn's and Colitis
Organization (ECCO). In order to participate, please register in
advance here to obtain a local or toll-free phone number and your
personal pin. A live webcast of the call will also be available on
Teva's website
at: https://ir.tevapharm.com/Events-and-Presentations.
Following the conclusion of the call, a replay of the webcast will
be available within 24 hours on Teva's website.
About Inflammatory Bowel
Disease
UC and CD, the two main types of IBD, are chronic inflammatory
conditions of the GI tract resulting in debilitating and persistent
symptoms such as abdominal pain, diarrhea, rectal bleeding, fatigue
and weight loss.5,6 Prolonged inflammation can lead to damage
within the GI tract, including fibrosis, a common complication of
IBD characterized by an accumulation of scar tissue in the
intestinal wall, which may cause narrowing and obstruction often
requiring hospitalization and surgery. There is currently no
cure for IBD – the goal of treatment is to induce and maintain
remission and prevent flares.7
About the RELIEVE UCCD Phase 2b
Study
RELIEVE UCCD was a 14-week Phase 2b, randomized, double-blinded,
dose-ranging study to determine the efficacy, safety,
pharmacokinetics, and tolerability of duvakitug in adults with
moderate-to-severe ulcerative colitis (UC) or Crohn’s disease (CD).
The study was an innovative and efficient basket study design
allowing the inclusion of patients with either type UC and CD. It
is also the first and only randomized, blinded and
placebo-controlled Phase 2 study to investigate the impact of TL1A
in CD.
In the study, patients who met pre-specified inclusion criteria
were randomized to receive one of two duvakitug doses or placebo,
administered every two weeks subcutaneously, in a 1:1:1 ratio for
each indication (UC or CD) stratified by previous exposure to
advanced IBD therapies [yes (either biologics/small molecule) or
no] for 14 weeks. The UC cohort comprised adults with moderately to
severely active disease with inadequate response, loss of response
or intolerance to previous conventional and/or advanced therapies
(ATs). The CD cohort comprised adults with moderately to severely
active disease with documented inadequate response, loss of
response or intolerance to conventional and/or advanced therapies
(ATs).
Primary efficacy endpoints are the number of participants who
show clinical remission (as defined by the modified Mayo score) in
the UC cohort or the number of participants who show endoscopic
response (as defined by the SES-CD endoscopic score for CD) in the
CD cohort. The study includes sites in the U.S., Europe, Israel,
and Asia.2,3
About
Duvakitug
Duvakitug is a potential best-in-class human IgG1-λ2 monoclonal
antibody that targets tumor necrosis factor (TNF)-like ligand 1A
(TL1A), also known as TNF superfamily member 15 (TNFSF15). TL1A
signaling is believed to amplify inflammation and drive fibrosis
associated with inflammatory bowel disease (IBD) through binding
its receptor, death receptor 3 (DR3).
Duvakitug is uniquely designed to inhibit preferentially TL1A
signaling via DR3, with the potential advantage of reduced
TL1A-DcR3 inhibition.8
Duvakitug is currently in a Phase 2b clinical study for the
treatment of ulcerative colitis (UC) and Crohn’s disease (CD), the
two most common types of IBD. The safety and efficacy of duvakitug
have not been reviewed by any regulatory authority.
About the Teva and Sanofi
Collaboration
Teva and Sanofi are collaborating to co-develop and
co-commercialize Teva’s duvakitug for the treatment of UC and CD.
Each company will equally share the development costs globally, and
the net profits and losses in major markets, with other markets
subject to a royalty arrangement. Sanofi will lead the Phase 3
clinical development program. Teva will lead commercialization of
the product in Europe, Israel and specified other countries, and
Sanofi will lead commercialization in North America, Japan, other
parts of Asia and the rest of the world.
About Teva
Teva Pharmaceutical Industries Ltd. (NYSE and TASE: TEVA) is a
different kind of global pharmaceutical leader, one that operates
across the full spectrum of innovation to reliably deliver
medicines to patients worldwide. For over 120 years, Teva’s
commitment to bettering health has never wavered. Today, the
company’s global network of capabilities enables its 37,000
employees across 57 markets to advance health by developing
medicines for the future while championing the production of
generics and biologics. If patients have a need, we’re already
working to address it. To learn more about how Teva is all in for
better health, visit www.tevapharm.com.
About Sanofi
We are an innovative global healthcare company,
driven by one purpose: we chase the miracles of science to improve
people’s lives. Our team, across the world, is dedicated to
transforming the practice of medicine by working to turn the
impossible into the possible. We provide potentially life-changing
treatment options and life-saving vaccine protection to millions of
people globally, while putting sustainability and social
responsibility at the center of our ambitions. Sanofi is listed on
EURONEXT: SAN and NASDAQ: SNY.
Cautionary Note Regarding
Forward-Looking Statements
This press release contains forward-looking
statements within the meaning of the Private Securities Litigation
Reform Act of 1995, which are based on management’s current beliefs
and expectations and are subject to substantial risks and
uncertainties, both known and unknown, that could cause our future
results, performance or achievements to differ significantly from
that expressed or implied by such forward-looking statements. You
can identify these forward-looking statements by the use of words
such as “should,” “expect,” “anticipate,” “estimate,” “target,”
“may,” “project,” “guidance,” “intend,” “plan,” “believe” and other
words and terms of similar meaning and expression in connection
with any discussion of future operating or financial performance.
Important factors that could cause or contribute to such
differences include risks relating to: our ability to successfully
develop duvakitug (Anti-TL1A) for the treatment of ulcerative
colitis (UC) and Crohn’s disease (CD), including to proceed to
Phase 3 study and obtain required regulatory approvals; our ability
to successfully compete in the marketplace, including our ability
to develop and commercialize additional pharmaceutical products;
our ability to successfully execute our Pivot to Growth strategy,
including to expand our innovative and biosimilar medicines
pipeline and profitably commercialize the innovative medicines and
biosimilar portfolio, whether organically or through business
development, and to sustain and focus our portfolio of generic
medicines; the effectiveness of our patents and other measures to
protect our intellectual property rights; and other factors
discussed in our Annual Report on Form 10-K for the year ended
December 31, 2024, including in the sections captioned “Risk
Factors” and “Forward-looking Statements.” Forward-looking
statements speak only as of the date on which they are made, and we
assume no obligation to update or revise any forward-looking
statements or other information contained herein, whether as a
result of new information, future events or otherwise. You are
cautioned not to put undue reliance on these forward-looking
statements.
*P-values reported are one-sided at a
significance level of 0.10.mMS = modified Mayo Score; MES = Mayo
Endoscopic Subscore; HEMI = Histological-Endoscopic Mucosal
Improvement; SES-CD = Simple Endoscopic Score for Crohn’s Disease;
CDAI = Crohn’s Disease Activity Index; PRO2 = 2-item
Patient-Reported Outcome_____________________
- Reinisch, W., Stepek, D., Kempinski, R., Danese, S., Sands,
B.E., Ratiu-Duma, B., Singh, R., Barkay, H., Raphael, G., Jairath,
V. (2025, February 19-22). Duvakitug (TEV-48574), an anti-TL1A
monoclonal antibody, demonstrates efficacy and favourable safety as
an induction treatment in adults with moderately to severely active
ulcerative colitis: Results from a phase 2b, randomised,
double-blind, placebo-controlled, dose-ranging, basket trial
(RELIEVE UCCD) [Presentation OP40]. ECCO 2025, Berlin,
Germany.
- A Study to Evaluate the Long-Term Effect of TEV-48574 in
Moderate to Severe Ulcerative Colitis or Crohn’s Disease.
https://clinicaltrials.gov/study/NCT05668013?term=TEV-48574&rank=1.
Accessed February 2025.
- A Study to Test the Effect of TEV-48574 in Moderate to Severe
Ulcerative Colitis or Crohn’s Disease (RELIEVE UCCD)
https://clinicaltrials.gov/study/NCT05499130?term=TEV-48574&rank=2.
Accessed February 2025.
- Jairath, V., Kierkuś, J., Duvall, G.A., Danese, S. Sands, B.E.,
Ratiu-Duma, B., Singh, R., Barkay, H., Raphael, G., Reinisch, W.
(2025, February 19-22). Duvakitug (TEV-48574), an anti-TL1a
monoclonal antibody, demonstrates efficacy and favourable safety as
an induction treatment in adults with moderately to severely active
Crohn’s disease: results from a phase 2b, randomised, double-blind,
placebo-controlled dose-ranging, basket trial (RELIEVE UCCD)
[Presentation OP41]. ECCO 2025, Berlin, Germany.
- Inflammatory Bowel Disease (IBD) Basics. Centers for Disease
Control and Prevention. 2022. Available at:
https://www.cdc.gov/inflammatory-bowel-disease/about/?CDC_AAref_Val=https://www.cdc.gov/ibd/what-is-IBD.html.
Accessed February 2025.
- Ulcerative Colitis Basics. Centers for Disease Control and
Prevention. 2024.
https://www.cdc.gov/inflammatory-bowel-disease/about/ulcerative-colitis-uc-basics.html.
Accessed February 2025.
- McDowell, C., Farooq, U., & Haseeb, M. (2020). Inflammatory
Bowel Disease (IBD). PubMed; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK470312/. Accessed February
2025.
- Clarke AW, et al. MAbs 2018;10(4):664-677. 2. Angeles T, et al.
UEGW.
Sanofi (EU:SAN)
Gráfico Histórico do Ativo
De Jan 2025 até Fev 2025
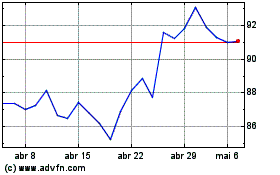
Sanofi (EU:SAN)
Gráfico Histórico do Ativo
De Fev 2024 até Fev 2025
